As the White House continues to pay lip service regarding the need to address our nation’s growing opioid epidemic, its policy does the opposite — stripping resources from the very programs working to address the crisis.
The Trump Administration has relentlessly attacked and sabotaged Medicaid, which helps people with opioid addiction receive care, paying for one-fifth of all substance abuse treatment nationwide. Beyond slashing funds for Medicaid, Trump has also encouraged states to impose burdensome work requirements, mandating that Medicaid enrollees work a set amount of hours each week and jump through administrative hurdles to prove their employment status. Adding insult to injury, the Trump Administration has proposed a 95% cut to the Office of National Drug Control Policy, which is charged with coordinating the federal response to the nation’s raging opioid crisis – a cut proposed for the second year in a row.
These policies are counterproductive at best, cruel and life-threatening at worst. Medicaid has played a central role in responding to the opioid epidemic, and cutting access will only make it harder for states to address the crisis.
MEDICAID GIVES STATES MORE RESOURCES TO ADDRESS THE OPIOID EPIDEMIC
Medicaid Is A Sustainable Source Of Funding Compared To Short-Term Grants. “Now that more people with SUDs are eligible for Medicaid, states can significantly improve treatment for people with SUDs by improving Medicaid-covered services. Medicaid can be a sustainable funding source for providers, as opposed to capped, short-term grant funding.” [Center on Budget and Policy Priorities, 2/28/18]
Thanks To Medicaid Expansion, The Uninsured Rate For Opioid-Related Hospitalizations Dropped In Expansion States. “In Medicaid expansion states, the uninsured rate for opioid-related hospitalizations plummeted by 79 percent, from 13.4 percent in 2013 (the year before expansion implementation) to 2.9 percent in 2015. The decline in non-expansion states was a much more modest 5 percent, from 17.3 percent in 2013 to 16.4 percent in 2015.” [Center on Budget and Policy Priorities, 2/28/18]
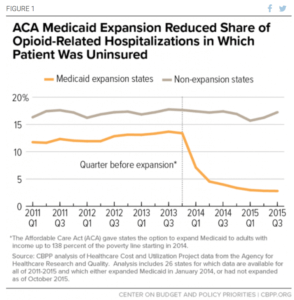
[Center on Budget and Policy Priorities, 2/28/18]
MEDICAID EXPANSION HAS INCREASED ACCESS TO TREATMENT
Medicaid Helps Make Buprenorphine And Naloxone, Drugs Used To Treat Opioid Use Disorder, Affordable. “These data are consistent with other evidence that Medicaid expansion is improving access to care for people with opioid use and other substance use disorders. Medicaid makes medications like buprenorphine and naloxone, which are prescribed to combat opioid use disorders, affordable for beneficiaries.“ [Center on Budget and Policy Priorities, 2/28/18]
Medicaid Expansion Has Improved Access To Substance Treatment Services. “Evidence also suggests that Medicaid expansion improved access to substance use treatment services more broadly. After expanding Medicaid, Kentucky experienced a 700 percent increase in Medicaid beneficiaries using substance use treatment services. Use of treatment services rose nationally as well; one study found that expanding Medicaid reduced the unmet need for substance use treatment by 18.3 percent.” [Center on Budget and Policy Priorities, 2/28/18]
In Ohio, Medicaid Has Helped Those With Substance Use Disorders Access Mental Health Services. “An Ohio study found that 59 percent of people with opioid-use disorders who had gained Medicaid coverage under expansion reported improved access to mental health care. Nationwide, the share of people forgoing mental health care due to cost fell by about one-third as the ACA, including Medicaid expansion, took effect.” [Center on Budget and Policy Priorities, 2/28/18]
THE REPUBLICAN CLAIM THAT MEDICAID CONTRIBUTED TO THE OPIOID EPIDEMIC IS FALSE
PolitiFact: “No evidence to prove Medicaid expansion is fueling the opioid crisis.” [PolitiFact, 10/23/17]
CBPP: States That Have Expanded Medicaid Have Reduced Unmet Need For Substance Abuse Treatment. “Expansion states have reduced the unmet need for the treatment of substance use disorders by 18 percent. All states’ Medicaid programs cover at least one medically assisted treatment medication, and the Medicaid expansion has granted health coverage to an estimated 99,000 people with an opioid use disorder.” [Center on Budget and Policy Priorities, 10/5/17]
Opioid Deaths In Medicaid Expansion States Predates The Affordable Care Act. “The opioid epidemic started decades before Medicaid expanded … Expansion states did have relatively more drug deaths than non-expansion states in 2015, but the upward trend in deaths in expansion states started in 2010, four years before the Medicaid expansion began. The results are the same if we exclude the six early expansion states. By the simplest criterion for causality, that causes must precede effects, these results cannot be taken as evidence of Medicaid expansion causing these deaths.” [Health Affairs, 8/23/17]
Medicaid Is Part Of The Solution To Curbing Opioid Epidemic. “Medicaid is the most powerful vehicle available to states to fund coverage of prevention and treatment for their residents at risk for or actively battling opioid addiction….The greatest opportunity to address this crisis is in those states that have elected to expand Medicaid, given the greater reach of the program, additional tools available, and the increased availability of federal funds.” [State Health Reform Assistance Network, 7/16]
CDC: “There Is No Evidence Medicaid Leads To Opioid Abuse.” “The Republican argument is flawed because the Medicaid expansion began in 2014, and opioid addiction was declared an epidemic by the Centers for Disease Control and Prevention in 2011. The federal science agency has also said there is no evidence that Medicaid leads to opioid abuse.” [Newsweek, 1/17/18]
Vox: “This Claim Runs Into A Basic Problem: The Concept Of Time.” “But this claim runs into a basic problem: the concept of time. Medicaid didn’t expand under Obamacare until 2014 — well after opioid overdose deaths started rising (in the late 1990s), after the Centers for Disease Control and Prevention in 2011 declared the crisis an epidemic, and as the crisis became more about illicit opioids, such as heroin and fentanyl, rather than conventional opioid painkillers. ‘It’s pretty ridiculous,’ Andrew Kolodny, an opioid policy expert at Brandeis University who’s scheduled to testify at the Senate hearing, told me.” [Vox, 1/17/18]
David Wyman, Georgetown University Law Center: “Just Because A Precedes B Doesn’t Mean That A Causes B. That’s Statistics 101.” “The witnesses included one anti-Medicaid ideologue, two local prosecutors who testified that they’ve seen a lot of addicts in their work and lots of them seem to be on Medicaid, and two experts who, tactlessly, pointed out that the causes of the opioid epidemic are many and complex, that it started years before Medicaid expansion, and that it involves patients and doctors in Medicare and private insurance as well as the uninsured… Efforts to demonize Medicaid expansion because it was launched as the opioid crisis really took off confuse correlation with causation, David Hyman of the Georgetown University Law Center warned Johnson’s committee. ‘Just because A precedes B doesn’t mean that A causes B,’ he said. ‘That’s statistics 101.’” [Los Angeles Times, 1/17/18]
Katherine Baicker, University Of Chicago Harris School Of Public Policy Dean: “I Don’t Think Anybody Would Suggest Because Overprescribing Of Opioids Poses A Series Health Risk, People Shouldn’t Go See The Doctor.” “If [Republicans] argue against Medicaid based on the idea that it potentially allows more patients to get prescriptions for opioids, they could use that same reasoning to oppose expansion of private health insurance. Expanding health insurance of any variety increases people’s access to health care. Much of that care is beneficial; some may not be, Katherine Baicker, dean of the University of Chicago’s Harris School of Public Policy, told me. ‘I don’t think anybody would suggest because overprescribing of opioids poses a series health risk, people shouldn’t go see the doctor,’ Baicker said.” [Washington Post, 1/17/18]
THOSE WHO ARE MOST FAMILIAR WITH THE OPIOID CRISIS AGREE THAT MEDICAID IS CRUCIAL IN FIGHTING IT
A Panel Of Public Health Officials, Policy Experts, And Law Enforcement Officials Found Medicaid Among Most Important Programs In Combating Opioid Epidemic. Investing in Medicaid was the third most cited response when a panel of thirty experts were asked where they would put money to combat the opioid epidemic. [New York Times, 2/14/18]
Jay Unick, University Professor: Medicaid Expansion Is Most Important Intervention To Improve Opioid Epidemic. Medicaid expansion would be “the most important intervention for improving outcomes related to the opiate epidemic…all the other interventions discussed here only work if individuals have access to quality health care.” [New York Times, 2/14/18]
160 National, State, and Local Organizations Warn That Trump’s Medicaid Sabotage Will Hurt Those With Substance Use Disorders in Letter to Secretary Azar: “CMS’s Medicaid work requirements policy is directly at odds with bipartisan efforts to curb the opioid crisis…and will have a significant and disproportionately harmful effect on individuals with chronic health conditions, especially those struggling with substance use disorders (SUDs) and mental health disorders.” [Letter, 2/15/18]
Signatories include: ADAP Advocacy Association (aaa+); Addiction Policy Forum, Advocacy Center of Louisiana; AIDS United, Alameda County Community Food Bank; American Association on Health and Disability; American Association of People with Disabilities; American Association for the Treatment of Opioid Dependence (AATOD); American Civil Liberties Union; American Federation of State; County & Municipal Employees (AFSCME); American Foundation for Suicide Prevention; American Group Psychotherapy Association; American Psychological Association; American Society of Addiction Medicine; Association for Ambulatory Behavioral Healthcare; Bailey House, Inc.; Board for Certification of Nutrition Specialists; Brooklyn Defender Services; CADA of Northwest Louisiana; California Consortium of Addiction Programs & Professionals; California Hepatitis Alliance; Caring Across Generations; Caring Ambassadors Program; CASES; Center for Civil Justice; Center for Employment Opportunities (CEO); Center for Health Law and Policy Innovation; Center for Law and Social Policy (CLASP); Center for Medicare Advocacy; Center for Public Representation; Charlotte Center for Legal Advocacy; CHOW Project; Coalition of Medication Assisted Treatment Providers and Advocates; Colorado Center on Law and Policy; Community Access National Network (CANN); Community Catalyst; Community Health Councils; Community Legal Services of Philadelphia; Community Oriented Correctional Health Services; Community Service Society; Connecticut Legal Services; Consumer Health First; C.O.R.E. Medical Clinic, Inc.; Council on Social Work Education; CURE (Citizens United for Rehabilitation of Errants); DC Coalition Against Domestic Violence; Desert AIDS Project; Disability Rights Arkansas; Disability Rights Wisconsin; Drug Policy Alliance; EAC Network (Empower Assist Care); EverThrive Illinois; Facing Addiction with NCADD; Faces & Voices of Recovery; FedCURE; First Focus; Florida Health Justice Project, Inc.; Food & Friends; The Fortune Society; Forward Justice; Friends of Recovery – New York; Futures Without Violence; God’s Love We Deliver; Greater Hartford Legal Aid; Greenburger Center for Social and Criminal Justice; Harm Reduction Coalition; Health Law Advocates; Hep Free Hawaii; Hepatitis C Support Project/HCV Advocate; Heartland Alliance; HIV Medicine Association; Horizon Health Services; Hunger Free America; ICCA; Illinois Association of Behavioral Health; The Joy Bus; JustLeadershipUSA; Katal Center for Health, Equity, and Justice; The Kennedy Forum; Kentucky Equal Justice Center ; Kitchen Angels ; Justice in Aging ; Justice Consultants, LLC; Lakeshore Foundation; Law Foundation of Silicon Valley; Legal Action Center; The Legal Aid Society; Legal Council for Health Justice; Life Foundation; Live4Lali; Liver Health Connection; Maine Equal Justice Partners; MANNA (Metropolitan Area Neighborhood Nutrition Alliance); Massachusetts Law Reform Institute; McShin Foundation; Mental Health America; Mental Health Association in New York State, Inc. (MHANYS); Michigan Poverty Law Program; Minnesota Recovery Connection; Mississippi Center for Justice; NAACP; The National Alliance to Advance Adolescent Health; National Alliance on Mental Illness; NAMI-NYS; National Alliance of State & Territorial AIDS Directors; National Association of Addiction Treatment Providers; National Association of County Behavioral Health & Developmental Disability Directors; National Association for Rural Mental Health; National Association of Social Workers; National Center for Law and Economic Justice; National Coalition Against Domestic Violence; National Council on Alcoholism and Drug Dependence, Phoenix; National Council for Behavioral Health; National Council of Churches; National Disability Rights Network; National Employment Law Project; National Federation of Families for Children’s Mental Health; National Health Care for the Homeless Council; National Health Law Program; National HIRE Network; National Juvenile Justice Network; National LGBTQ Task Force; National Low Income Housing Coalition; National Organization for Women; The National Viral Hepatitis Roundtable; NC Justice Center; New Haven Legal Assistance Association; New York Association of Alcoholism and Substance Abuse; New York Association of Psychiatric Rehabilitation Services; New York Lawyers for the Public Interest; New York State Council for Community Behavioral Healthcare; Open Hands Legal Services; Osborne Association; Outreach Development Corp.; The Partnership for Drug Free Kids; PICO National Network; The Poverello Center, Inc.; Project Inform; Public Justice Center; Root & Rebound; Ryan White Medical Providers Coalition; Safer Foundation; Sargent Shriver National Center on Poverty Law; School Social Work Association of America; Sea Island Action Network, South Carolina; The Sentencing Project; Shatterproof; Society of General Internal Medicine; Southern Center for Human Rights; Southern Poverty Law Center; Students for Sensible Drug Policy; TASC of the Capital District, Inc.; Tennessee Justice Center; Three Square Food Bank; Transitions Clinic Network; Treatment Action Group; Treatment Alternatives for Safe Communities (TASC) – Illinois; Treatment Communities of America; Virginia Poverty Law Center; Western Center on Law & Poverty

