In a last-ditch effort to repeal the Affordable Care Act with only Republican votes before the September 30th deadline, Senators Lindsey Graham (R-SC), Bill Cassidy (R-LA), Dean Heller (R-NV) and Ron Johnson (R-WI) unveiled their latest proposal this week. While some may look at this effort as a Hail Mary pass with little chance to succeed, Sen. Cassidy said today that 48 or 49 Republican senators are on board with this bill, meaning they are only a couple of votes away from being able to pass the bill on the Senate floor.
The Graham-Cassidy-Heller-Johnson (GCHJ) bill would radically change our health care system — getting rid of the Affordable Care Act tax credits and Medicaid expansion and changing them into block grants with dramatically less funding for states. It would also convert traditional Medicaid into a per capita cap program. In short, this bill would slash coverage, raise costs, eliminate protections for millions of people across America, as well as gut Medicaid. In fact, it is potentially the worst of the repeal bills that we have seen to date.
Given Republicans will have to ram this partisan repeal bill through the Senate in the next two weeks in order to meet this September 30 deadline there will be no time for a regular process for the public to fully understand the impacts on their health care — with no time for adequate hearings, consultations with experts, constituent input, and amendments. Republicans in the Senate are resorting back to a secret, partisan process to force through health care repeal out of public view. — The American people need to know the facts about how this bill will impact them. Here are the top six (6) reasons why they should reject GCHJ just as they have rejected the previous repeal attempts.
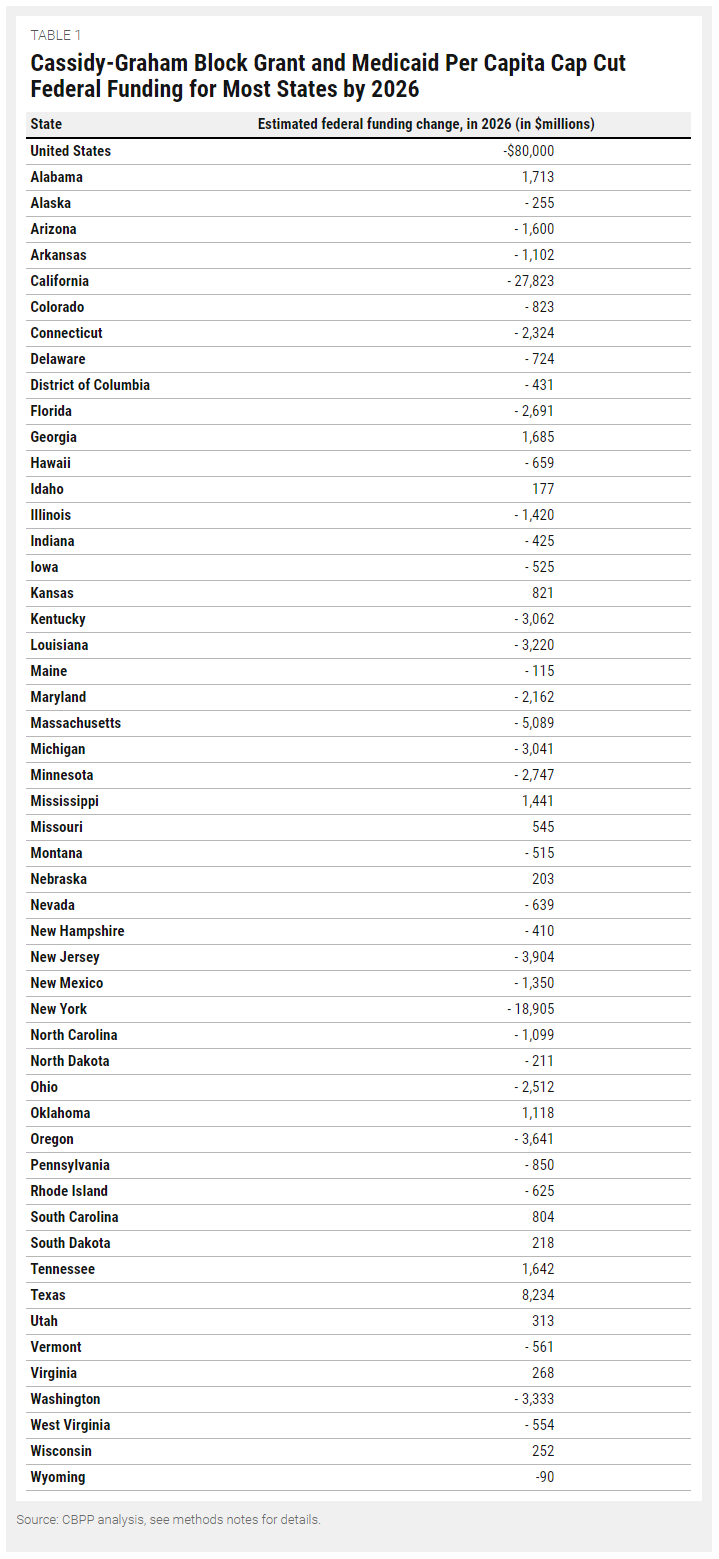
GCHJ Cuts Funding to Most States & Punishes States that Expanded Medicaid
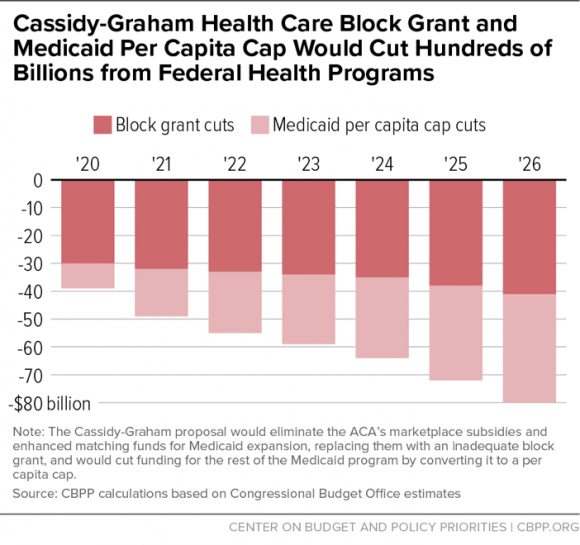
Overall, Graham-Cassidy-Heller-Johnson cuts spending on marketplace tax credits and Medicaid expansion and converts them into a block grant. Between 2020 and 2026, GCHJ would cut $239 billion from what was projected to be spent under current law for the tax credits and expansion. After 2026, the block grant funding is eliminated altogether. Moreover, GCHJ would convert traditional Medicaid into a per capita program and cut spending by another $175 billion from 2020 to 2026. This aspect is what makes GCHJ potentially the worst among all the partisan repeal bills.
The Center on Budget and Policy Priorities analyzed the latest Graham-Cassidy-Heller-Johnson proposal and found that all but twelve states would receive less federal funding. In 2026, Alaska would lose $255 million; Arizona, $1.6 billion; Louisiana, $3.2 billion; Maine, $115 million; Nevada, $639 million; Ohio, $2.5 billion; and West Virginia,
$554 million, just to name a few.
Source: Center on Budget and Policy Priorities, 9/13/17
Moreover, GCHJ’s state funding allocation redistributes funding to states that did not expand Medicaid at the expense of states that did. In other words, this bill punishes states that expanded Medicaid and chose to provide health coverage to more of their citizens. As the Center on Budget writes:
The block grant would not only cut overall funding for the Medicaid expansion and marketplace subsidies but also, starting in 2021, redistribute the reduced federal funding across states, based on their share of low-income residents rather than their actual spending needs. In general, over time, the plan would punish states that have adopted the Medicaid expansion or been more successful at enrolling low- and moderate-income people in marketplace coverage under the ACA. It would impose less damaging cuts, or even raise funding initially, for states that have rejected the Medicaid expansion or enrolled few low-income residents in marketplace coverage.
Source: Center on Budget and Policy Priorities, 9/13/17
GCHJ Would Slash Coverage
The billions of dollars in cuts to Medicaid and marketplace tax credits would result in millions of people losing health care coverage. For example, GCHJ ends Medicaid expansion, which has extended health coverage to 11 million low-income adults.
Another important point is that GCHJ ends block grant spending in 2026, or rather, spending for Medicaid expansion and marketplace tax credits. What that means is in 2026 GCHJ repeals the Affordable Care Act without a replacement. Earlier analyses showed a “repeal-without-replace” would result in 32 million people losing coverage and individual markets collapsing.
GCHJ Would Raise Health Care Costs
Graham-Cassidy-Heller-Johnson raises consumer health costs in a variety of ways. As discussed above, the bill would cut funding people get to help pay for premiums — through marketplace tax credits and by getting affordable coverage through Medicaid expansion.
According to the Brookings Institution, the result would be “that no one in a state’s individual market that waived EHBs would have access to comprehensive coverage. Insurers would likely sell separate policies for benefits not covered in their core plan offerings, but these supplemental policies would be subject to tremendous adverse selection, leading to very high premiums and enrollment almost exclusively by those with pre-existing conditions.” For example, a woman who purchases a separate insurance rider for maternity care would have to pay $17,320 more, according to the Center for American Progress. For states that no longer required substance use disorders or mental health to be covered, coverage for drug dependence treatment could cost an extra $20,450.
Allowing states to opt out of the essential health benefits coverage means that insurance companies could once again put lifetime and annual limits on the amount of care you receive. Moreover, this would even impact people with coverage from their employer. The Center for American Progress estimates that 20 million people with health coverage through their employer would face lifetime limits on coverage, and 27 million would face annual limits
GCHJ Would Gut Protections for People With Pre-Existing Conditions
The American Cancer Society Cancer Action Network said allowing states to waive essential health benefits “could render those protections meaningless” for people with pre-existing conditions.
The American College of Physicians called for regular order and wrote that “We believe that the substantial cuts to Medicaid authorized by this legislation would cause a significant increase in the number of uninsured patients and that it would undermine essential benefits provided for patients insured under current law.”
Consumers Union said that allowing states to waive essential health benefits would be “putting meaningful coverage out of reach for many Americans, especially those with chronic and pre existing conditions.” Because states could opt out of covering these basic benefits, insurers would likely only offer policies that covered much less than they do now. The Kaiser Family Foundation found that the benefits most likely to no longer be covered would be maternity care, mental health or substance abuse coverage.
Key Stakeholders Oppose GCHJ
On Wednesday, key health care stakeholders — including the American Academy of Family Physicians, American Academy of Pediatrics, American College of Physicians, the American Congress of Obstetricians and Gynecologists, the American Osteopathic Association and the American Psychiatric Association — sent a letter to the Senate opposing the Graham-Cassidy-Heller-Johnson bill saying it would “have a negative impact on affordable coverage for patients across our nation.” The groups urged the Senate to go through a regular order to find bipartisan solutions on health care.
In addition, the American Cancer Society Cancer Action Network said GCHJ “would be disruptive to the health care markets — creating uncertainty for millions of Americans.”
GCHJ Undermines Bipartisan Negotiations Underway
Last week, we saw Republicans and Democrats on the Senate Health, Education, Labor and Pensions (HELP) Committee, led by Senators Lamar Alexander (R-TN) and Patty Murray (D-WA), work together to find a solution to stabilize the individual market by making payments to help consumers lower out-of-pocket costs and deductibles. Insurers have cited the threat of defaulting on these payments-which the Trump administration has repeatedly threatened to do- as the main reason they would raise premiums or exit the markets. A bipartisan group of governors and insurance commissioners testified before the HELP Committee agreeing these payments needed to be made. The nonpartisan Congressional Budget Office concluded failure to make these payments would result in premiums skyrocketing 20 to 25 percent and adding nearly $200 billion to the federal debt.
The Graham-Cassidy-Heller-Johnson bill threatens this bipartisan work by once again injecting partisan repeal into the process for no reason.